Our Story
The 90 Degree
Benefits Advantage
90 Degree Benefits believes that delivering the future of health plans is about more than just providing benefits. We create peace of mind through our health plan offerings for employers which play a pivotal role in the success of their company.

Our Vision
To be a distinguished leader in the TPA industry, differentiating ourselves with benefit solutions for our clients’ continued success.
Our Mission
We serve our customers through collaborative and courageous actions in order to exceed expectations and continually strive for the best outcomes for employers and their employees.
Innovative Solutions
90 Degree Benefits serves as an innovative partner finding the right solutions for our customers' needs. In addition to major medical coverage, 90 Degree Benefits supports clients by developing and administering products for retirement plan assistance, ancillary coverage (including GAP and dental), pharmacy solutions (including GLP-1), legal/compliance advice, and a variety of claims administrative services. Year after year, client after client, 90 Degree Benefits finds new ways to ensure customer satisfaction.
90 Degree Benefits continues to grow by finding innovative solutions for our clients. In addition to traditional major medical plans, we've continued to support clients by expanding into retirement plan assistance, dental and GAP coverage, and a variety of claims administrative services.
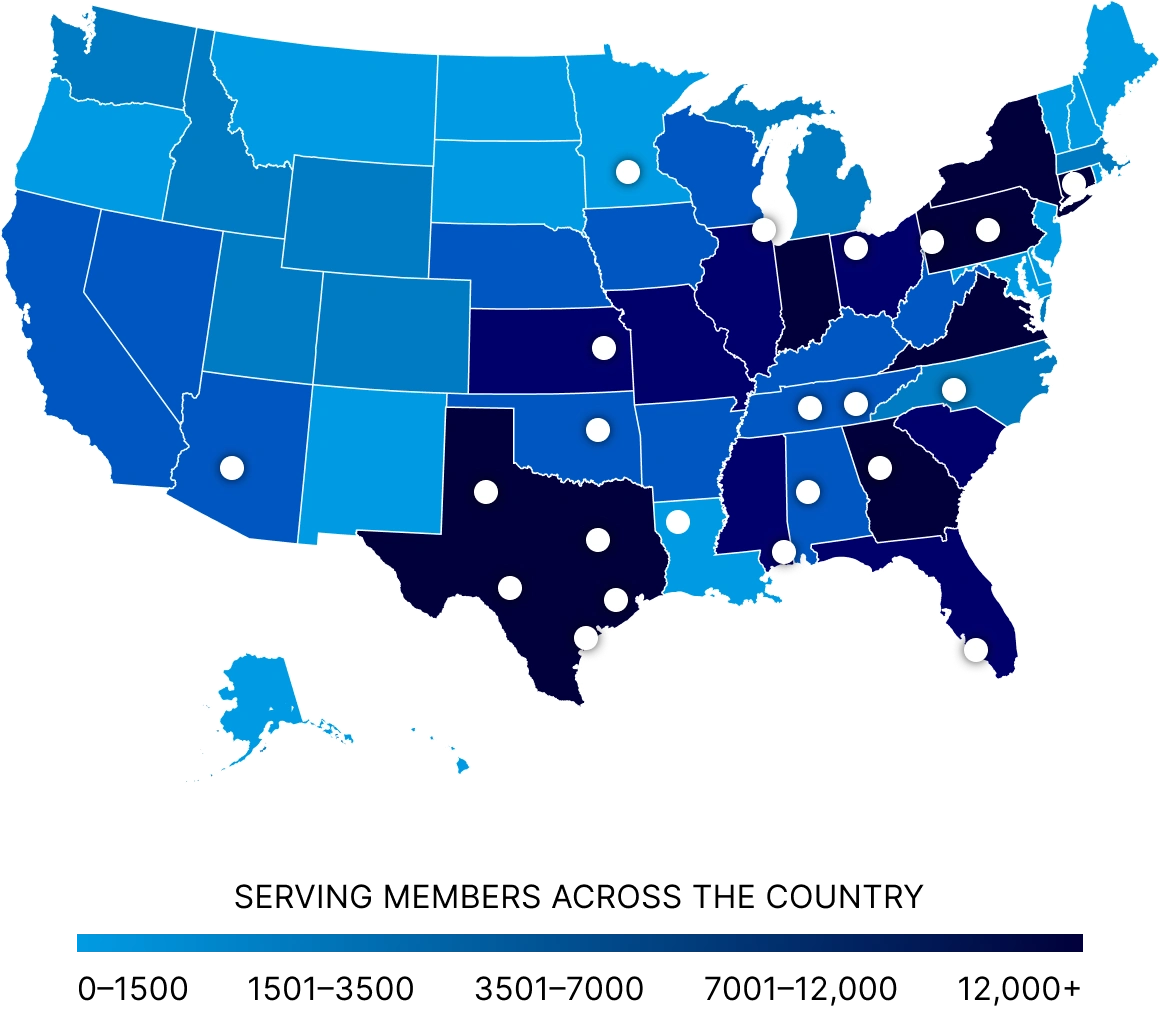
Today, 90 Degree Benefits touches 700,000 lives annually through our diverse portfolio of products and services.

Continual Growth. Perpetual Commitment.
We combine continuous innovation with a relentless focus on client success, delivering smarter health benefits solutions that drive better outcomes. Our commitment to progress ensures your plans are always one step ahead.
The Power of Partnership
Advancing the Future of Health Benefits
90 Degree Benefits has formed strategic partnerships to expand our solutions and provide industry-leading resources for our partners and clients. We are committed to shaping the future of healthcare through thoughtful collaboration.
90 Degree Benefits takes the challenges of a costly and complicated healthcare system and turns them into new opportunities and simple solutions for you and your clients.